The ugly truth about going gluten-free that nobody talks about : The Hearty Soul

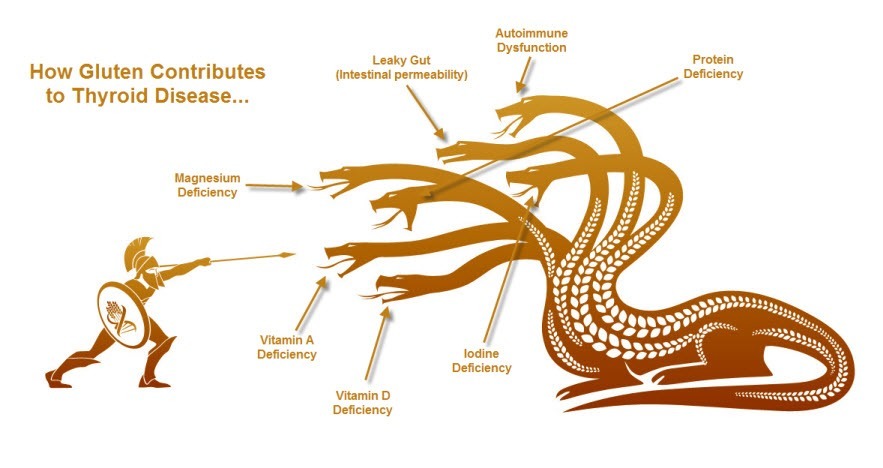
Going Gluten Free is a huge first step in improving your health, especially if you’ve been diagnosed with an autoimmune disease. BUT and this is a huge but, it may not be enough by itself… and here’s why:
Autoimmune Disease and Gluten
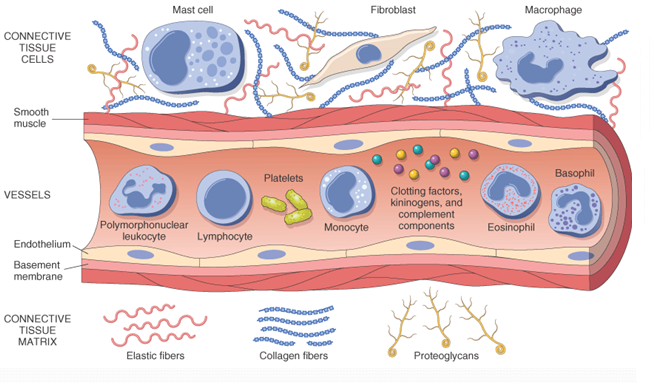
Autoimmunity is a complex disease where your body mistakes your own tissue as foreign and your white blood cells relentlessly attack it with the goal to destroy it! I’ve learned the hard way in treating both my wife and mother with Hashimoto’s just how complicated treatment can be. Because of this, I’ve put together a 10 day Guide to help those with Autoimmune disease.
The goal of everything you do to treat your autoimmune disease should be to reduce the inflammation in your body and the immune attack on your own tissue. If your treatment isn’t targeted at either of those, then you’re doing it wrong.
And that’s why going Gluten free works so well, right? Well, sort of…
Going gluten free is a step in the right direction for many people, because as you probably know gluten sensitivity means your body is sensitive to the gluten protein. You are probably already aware that there’s a huge crossover in people who have celiac’s disease AND autoimmune disease so why isn’t it enough to eliminate it from your diet?
Why Going Gluten-Free Isn’t Enough
Reason #1: You’re Doing it Wrong (you gave up gluten but kept in snacks and fake bread, you’re still eating hidden gluten and causing inflammation).

Don’t get down on yourself. You should be congratulated for even taking this step towards better health! But… The truth is that many people who go “gluten free” are actually doing it wrong.
Here are a few quick ways to know if you are doing gluten free the wrong way:
- You avoid bread, but you don’t look for gluten in other products (soy sauce, hot dogs, lipstick, toothpaste – these all have gluten in them!)
- You avoid sweets with gluten in them, but you still buy gluten free pastries, cake mixes, brownie mixes, ice cream, etc.
- You did a great job taking out gluten but you still aren’t eating vegetables! That’s 5-9 servings per day!
- You are gluten free 95% of the time but you make exceptions for your favorite foods – even though it makes your stomach hurt afterward!
- You went gluten free for 4 weeks but didn’t notice a difference so you went back to eating it again.
Does any of these sound familiar? If so you are probably doing gluten free the wrong way. Here’s the truth: In certain people, and not just those with Celiac’s disease, gluten is a highly inflammatory food.
That means it amps up your immune system and puts your body into a state of being hyper alert. During this stage, you’re now set up to accidentally attack your own body in what’s called autoimmunity. Gluten is, unfortunately, the ringleader in this process and that’s why it’s so critical to completely remove it from your body!
That Means:
- You must COMPLETELY avoid gluten for at least 3 months – a trial period of 1 month will not do it.
- Look for it everywhere and don’t make any assumptions – it’s hiding in the weirdest places (like the examples above).
- No cheating! Even a little bit of gluten amps your immune system back up in a hurry.
- Eating healthy means eating fruits and vegetables…
- That also means – gluten-free junk food is still just junk food.
Try out these recommendations before you make the assumption that going gluten free didn’t work for you.
Reason #2: You Have Other Gut Imbalances (SIBO, Dysbiosis, Gut infections, Yeast Overgrowth)
Ever wonder why you’re so prone to gut problems? Constipation, gas pains, abdominal pain, bloating, cramping…Patients with gluten sensitivity are predisposed to developing other gut issues due to inflammation. And it’s a big deal.
Patients with autoimmune diseases are more likely to have other gut issues like SIBO (small intestinal bacterial overgrowth), Intestinal Dysbiosis (too much bad bacteria and not enough good bacteria), Gut Infections (like parasites), Leaky Gut and Yeast Overgrowth.
These are serious issues that NEED to be taken care of, and going gluten free just simply isn’t enough to treat them. How do you know if you have these problems? A knowledgeable doctor can order advanced stool testing to diagnose many of these problems. If you don’t have access to a functional medicine doctor then you can do your own down and dirty testing by answering these questions:
- Was I still constipated on a gluten free diet?
- Did I still experience gas and bloating 30 minutes to 1 hour after a meal?
- Do I still have abdominal pain?
- Are my bowel movements still irregular? Diarrhea one day, constipation the next?
- Do I have a personal history of lots of antibiotic use as a child or adult?
- Do I still experience unusual reactions to certain foods? Rashes, hives, swelling under the eyelid or in my arms/legs?
If you answered yes to any of these questions then you likely have one or more of these gut related issues. You can trial some treatments but I would strongly recommend getting definitive testing and treatment.
Reason #3: Your Immune System is Still on Fire Because of Physical, Emotional or Physiologic Stress
It’s no secret that stress increases inflammation and activates your immune system. But what you may not have known is just how little stress can actually impact your entire body.
The truth is that the small amount of constant every-day stress that we all experience really takes a toll on both our bodies and our guts. I’m not talking the death of a loved one either (though that can take a HUGE toll). I’m talking about little stress: work stress, financial stress, family or marriage stress, social media stress, etc.
The little things day in and day out really add up over time to increase inflammation.There are plenty of scientific studies that prove stress can destroy your health, but if you don’t believe me just consider a few simple examples:
- Have you ever had diarrhea before a stressful event?
- Have you ever had a “gut feeling” about something?
- Have you ever had “butterflies” before?
I’m sure each one of you can connect with at least one of those examples and they all illustrate just how emotions and thoughts can affect your gut! But let’s get to the science… It’s clear that chronic low-grade stress (like the daily stress we all deal with) causes a number of negative changes in your gut:
- It can change the composition of your bacteria – in favor of bad bacteria.
- Stress increases intestinal permeability, A.K.A causes leaky gut.
- It has even been associated with an increased risk of GERD, peptic ulcer disease, inflammatory bowel disease (like Crohn’s and Ulcerative Colitis), irritable bowel syndrome and even food allergies.
Simply put…
You can’t address your autoimmune disease without addressing your stress levels. The science is clear and the patients who undergo a comprehensive treatment plan would agree with it.
Quick Tip for Stress Reduction: Spend 20 minutes per day doing something you LOVE. This can be yoga, meditation, spiritual prayer. One of my favorites is to take an Epsom salt bath with baking soda and lavender essential oil. It provides a healthy dose of magnesium while reducing cortisol levels from the lavender.
Reason #4: You’re NOT Avoiding Foods that Cross-React with Gluten or Directly Cause Inflammation by Themselves (Milk, Rice, Corn, Sesame and Gluten Free Oats)
Avoiding gluten should be your first step into healing your autoimmunity, but it can’t be your last. Unfortunately many foods cross react with the gliadin molecule (the part of gluten that people don’t tolerate). Put in simple terms: the protein of gliadin and of milk, corn, rice, sesame and gluten free oats looks so similar that your body can’t tell the difference.
Because of this, it may still react to these food groups causing a “sensitivity” and causing inflammation. Many of these foods also cause inflammation due to various other reasons. Take milk for instance:
Not only does it contain lactose (which many people don’t tolerate), but it also contains the protein casein which another group of people can’t tolerate. No matter how you slice it removing these foods for a short period of time is not only helpful but NECESSARY for some people to reduce inflammation and start their healing journey.
Quick Diet Tip: Pick a diet that avoids these major food groups along with gluten and keep with that diet for at least 3 months.
Reason #5: Autoimmune Diseases are Complex and Require a Multifaceted Approach to Treatment
The more I research about autoimmunity the more I’m continually blown away at just how complex this disease really is. Unless you’re dealing with it, or have someone close to you that is, it’s really hard to wrap your head around just how devastating this disease can be.
From the brain fog, constant fatigue, lack of mental clarity, unexpected weight gain, depression, and hair loss to the roller coaster that comes with seeing multiple doctors after being misdiagnosed and mismanaged for years.
I’ve come to realize that a comprehensive, multifaceted approach to treatment is not only recommended but required for optimal results.My recommended treatment plan includes 6 steps and each step is critical:
- Proper diet that is tailored to the individual and helps nourish the adrenals while focuses on nutrient deficiencies and reducing inflammation and autoimmunity
- Addressing gut health and gut imbalances that may be accelerating inflammation in the body and reducing absorption of critical nutrients
- Address adrenal status with adaptogens or glandular
- Replete nutrient deficiencies, including Iron, B12, Zinc, Selenium, Iodine, and Vitamin D3
- Finding the right medications (if indicated) for each individual
- Removing toxins that may be interfering with hormonal production or disrupting organ function
My goal is to spread information to help as many people as possible. If you know someone who is suffering from autoimmune disease please share this information with them so they can start to feel like themselves again and get their life back.

Sources
- Biesiekierski, Jessica R, and Julie Iven. “Non-coeliac gluten sensitivity: piecing the puzzle together.” United European gastroenterology journal 3.2 (2015): 160-165.
- Barton, Susan H, and Joseph A Murray. “Celiac disease and autoimmunity in the gut and elsewhere.” Gastroenterology Clinics of North America 37.2 (2008): 411-428.
- Chang, Matthew S, and Peter HR Green. “A review of rifaximin and bacterial overgrowth in poorly responsive celiac disease.” Therapeutic advances in gastroenterology (2011): 1756283X11422264.
- Segerstrom, Suzanne C, and Gregory E Miller. “Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry.” Psychological bulletin 130.4 (2004): 601.
- Lyte, Mark, Lucy Vulchanova, and David R Brown. “Stress at the intestinal surface: catecholamines and mucosa–bacteria interactions.” Cell and tissue research 343.1 (2011): 23-32.
- Konturek, PC, T Brzozowski, and SJ Konturek. “RECHERCHER DANS LE BLOG.” Journal of Physiology and Pharmacology 62.6 (2011): 591-599.
- Konturek, PC, T Brzozowski, and SJ Konturek. “RECHERCHER DANS LE BLOG.” Journal of Physiology and Pharmacology 62.6 (2011): 591-599.
- Atsumi, Toshiko, and Keiichi Tonosaki. “Smelling lavender and rosemary increases free radical scavenging activity and decreases cortisol level in saliva.” Psychiatry Research 150.1 (2007): 89-96.